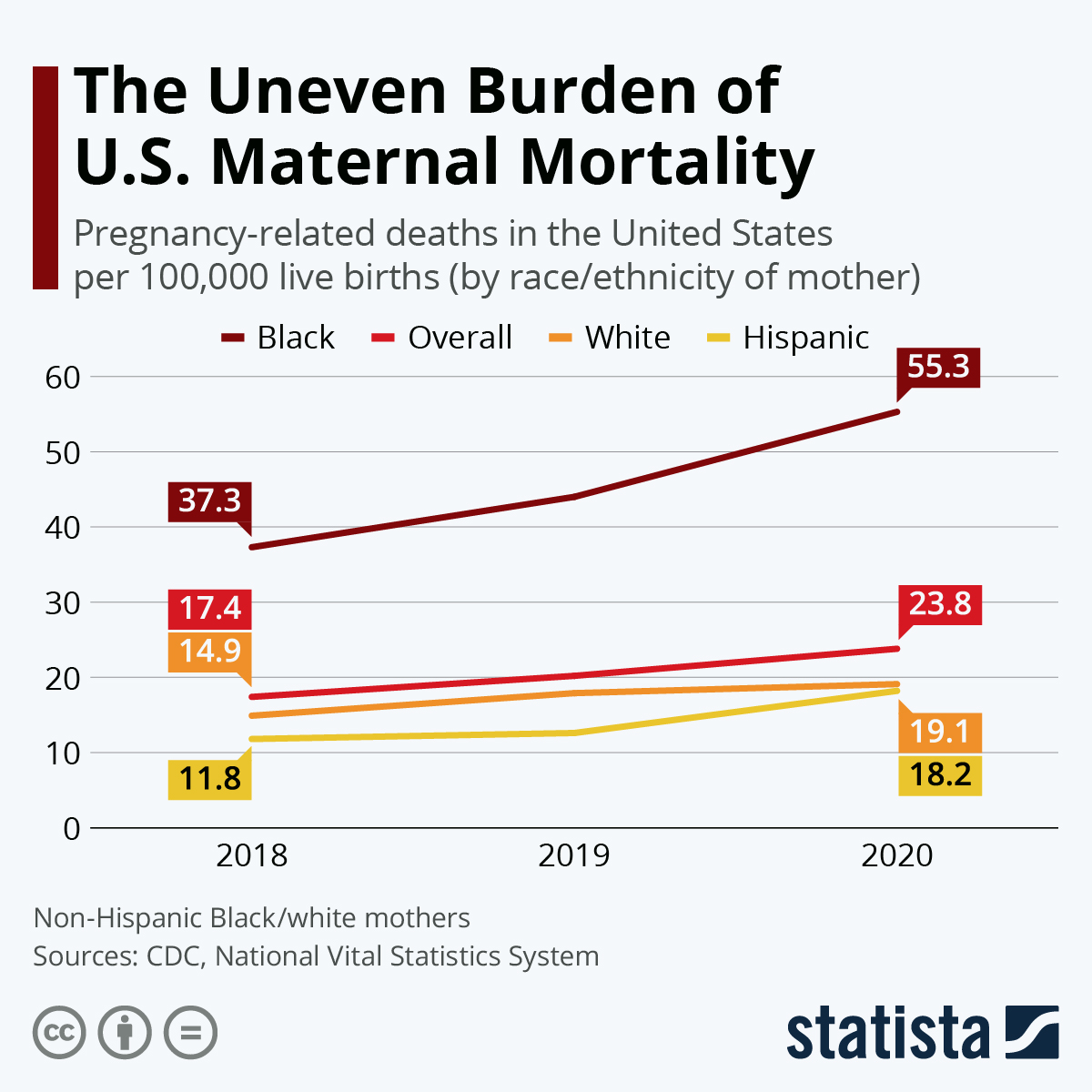
U.S. Maternal Mortality Rates Continue to Rise Alarmingly
U.S. maternal mortality continues to be a pressing public health issue, raising alarms as the nation leads other high-income countries in pregnancy-related deaths. Despite the fact that over 80% of these losses are preventable, significant gaps in maternal health care persist, exacerbated by alarming racial disparities in maternal health. Recent studies reveal an ongoing rise in the maternal mortality rate from 2018 to 2022, with stark variations across states and demographic groups. Access to quality prenatal and postpartum care plays a critical role in mitigating these risks, yet many women lack the comprehensive support needed during and after pregnancy. Addressing the alarming trend of preventable maternal deaths is imperative if we are to safeguard the health of mothers and their children in the United States.
The challenges surrounding U.S. maternal mortality highlight a systemic crisis in pregnancy and postpartum care, often referred to as maternal health disparities. These disparities not only reflect the urgent necessity for improved healthcare policies but also call attention to the higher rates of maternal death among particular racial groups. As we analyze the recent findings on pregnancy-related deaths, it becomes evident that there is an urgent need for equitable access to comprehensive maternal health services. The situation demands a multi-faceted approach to alleviate the preventable deaths that disproportionately affect marginalized communities. Ensuring that all expectant and new mothers receive quality care is essential for reversing the disturbing trends we observe in maternal health.
Understanding U.S. Maternal Mortality Rates
The U.S. continues to grapple with alarmingly high maternal mortality rates, surpassing those of other high-income countries. As indicated by recent studies, a significant proportion of these deaths—over 80%—are deemed preventable. This stark reality highlights ongoing challenges within the U.S. healthcare system, including fragmented care, inequitable access to maternal health services, and a lack of attention to chronic health conditions impacting pregnant individuals. The alarming trend is exacerbated by systemic issues such as biases in treatment and care delivery, particularly for women of color. Thus, addressing these disparities requires not only a commitment to improving healthcare policy but also a fundamental shift in how maternal health care is perceived and provided in the U.S.
Moreover, varying state-level statistics illustrate the troubling inconsistencies in maternal health care across the nation. For instance, a remarkably high maternal mortality rate for American Indian and Alaska Native women starkly contrasts with their white counterparts, emphasizing the need for targeted interventions to address these racial disparities. Recognizing effective models, such as those in California, could serve as a blueprint for other states striving to reduce their maternal mortality rates and improve overall health care for mothers.
Public health experts contend that the overarching issue lies within the structure of American maternal health care. The inadequacies of the system, characterized by maternity care deserts and insufficient postpartum resources, result in barriers that disproportionately affect marginalized groups. It is vital to confront these challenges head-on; only then can effective solutions emerge that prioritize maternal well-being. With growing evidence linking chronic health conditions like cardiovascular diseases to rising maternal deaths, comprehensive care that addresses these underlying factors is essential in bringing about meaningful change.
The Impact of Racial Disparities on Maternal Health
Racial disparities in maternal health care starkly manifest in the ongoing maternal mortality crisis in the U.S. Women of color, particularly non-Hispanic Black and American Indian women, experience significantly higher rates of pregnancy-related deaths compared to their white peers. These disparities reflect broader systemic issues that affect access to quality maternal health services, timely interventions during pregnancy, and effective postpartum care. Health disparities can be attributed to a complex interplay of social determinants, including economic stability, healthcare access, and systemic racism within the healthcare system, all contributing to the prevalence of preventable maternal deaths in these populations.
Furthermore, the persistence of these inequities calls for a multifaceted approach to maternal health policy reform. Initiatives must address both clinical care improvements and broader societal factors, such as health education, stable housing, and access to nutritional resources, which directly impact maternal and infant health outcomes. By implementing comprehensive strategies that consider the unique barriers faced by different racial and ethnic groups, we can begin to dismantle the systemic inequities that continue to plague maternal healthcare in the U.S.
Recent analysis underscores the need for inclusion of late maternal deaths—those occurring between 42 days and one year postpartum—in discussions around maternal mortality. This shift acknowledges that maternal health does not simply conclude at the six-week postpartum visit mandated by many healthcare systems. The growing acknowledgment of the importance of extended postpartum care is crucial since a significant number of deaths occur during this timeframe. Therefore, enhancing care continuity and support during the initial year after childbirth can be instrumental in addressing racial disparities in maternal health.
Challenges in Postpartum Care and Maternal Health Outcomes
Despite the strong emphasis on prenatal care, postpartum care has garnered less attention, often leading to suboptimal health outcomes for mothers. The problem of late maternal deaths points to a critical gap in our healthcare system, where the focus frequently shifts away from women after childbirth. Immediate postpartum care is essential, yet many women, especially from marginalized communities, face barriers in accessing necessary healthcare services. Improved postpartum care that includes routine check-ups and comprehensive support is vital in preventing complications that can arise during the first year after delivery.
The evidence suggests that a significant number of postpartum complications are preventable with proper care and monitoring. For example, conditions such as postpartum depression, hypertension, and other chronic diseases can severely impact maternal health if not properly addressed. There is an urgent need to elevate the conversation around postpartum health care, so mothers receive the continuous support and care needed for a healthy recovery. Acknowledging that postpartum care should extend well beyond the traditional six-week follow-up could significantly reduce the rates of preventable maternal deaths.
Innovative Solutions for Improving Maternal Health Care
To address the rising rates of maternal mortality in the U.S., innovative solutions and policy changes are paramount. Strategies such as expanding access to telehealth services, community health workers, and maternal care programs tailored to specific cultural needs can make a significant difference. Such interventions focus on creating supportive networks and resources that cater specifically to the unique challenges faced by diverse communities. By investing in these programs, we can ensure that all women, regardless of their race or economic status, receive the maternal care they need.
Moreover, enhancing staff training on implicit biases and culturally competent care can create a more understanding environment for women of color, who often report feeling overlooked or misunderstood within the healthcare system. Incorporating feedback from the very communities affected by maternal mortality can also guide health interventions, making them more relevant and effective. Ultimately, a collaborative effort between health care providers, policymakers, and community organizations is essential for developing lasting solutions that promote equitable maternal health outcomes.
The Role of Public Health Infrastructure in Maternal Mortality
Investing in public health infrastructure is critical in combating the rising rates of maternal mortality in the U.S. Currently, the fragmented health care system lacks uniformity, with many areas facing significant gaps in maternity care services. A robust public health framework can facilitate better tracking of maternal mortality data, ensuring that these statistics inform state-level policies that directly affect maternal health care quality. Accessible public health initiatives can serve as a foundation for preventive measures and education surrounding maternal health, ultimately leading to improved outcomes.
Moreover, funding for maternal health initiatives must be prioritized to combat the potentially dire consequences of budget cuts and deprioritization of maternal issues. Policymakers should recognize the long-term benefits of investing in maternal health, as supporting mothers during pregnancy and postpartum leads not only to healthier mothers but also to healthier children and families. Efforts to bolster public health infrastructure around maternal health must include a focus on community engagement and education, ensuring that all stakeholders play a role in promoting safe pregnancies and maternal well-being.
The Importance of Tracking Maternal Deaths
The lack of consistent tracking of maternal deaths in the U.S. has long hindered efforts to address maternal mortality effectively. The recent implementation of a standardized pregnancy checkbox on death certificates has provided a clearer picture, yet it remains a relatively recent development. Comprehensive tracking is essential to understanding the causes of maternal deaths and developing targeted interventions. Comprehensive data collection helps identify trends, risk factors, and demographic disparities in maternal health, guiding health policies and resources where they are needed most.
Furthermore, enhancing data collection processes can shed light on the factors contributing to late maternal deaths and facilitate a more nuanced approach to care. For instance, tracking mortality rates beyond 42 days postpartum can illuminate critical issues that require ongoing attention and intervention. By focusing on thorough and systematic tracking of maternal deaths, health administrations can ensure that public health strategies are data-driven, align with the needs of diverse maternal populations, and ultimately work towards reducing preventable maternal deaths.
Addressing the Impact of Chronic Conditions on Maternal Health
Chronic conditions have emerged as a leading concern in discussions about maternal health, particularly as they relate to rising rates of pregnancy-related deaths. Conditions such as hypertension, diabetes, and cardiovascular disease have shown significant increases among reproductive-age individuals. These growing health challenges underscore an urgent need for health systems to better recognize and manage chronic diseases in pregnant individuals. Increased pre-pregnancy care focused on managing these conditions can contribute immensely to improving maternal health outcomes.
Strategies that promote early diagnosis and treatment of chronic health conditions in women can lead to healthier pregnancies and improved maternal outcomes. Healthcare providers should prioritize integrating chronic disease management into routine prenatal care, providing patients with necessary resources and education to take charge of their health. By addressing chronic conditions effectively, the prevention of pregnancy-related deaths becomes more attainable, ensuring that all mothers receive the safe and quality care they deserve throughout their pregnancy journey.
Future Directions for Maternal Health Policies
As more data comes to light regarding maternal mortality in the U.S., it’s clear that future maternal health policies must be comprehensive, equitable, and sustainable. A personalized approach that considers the unique circumstances of various demographics, particularly women of color, is essential. Policymakers must commit to addressing the factors that contribute to health disparities while fostering a health care system that prioritizes maternal well-being. Collaborative efforts between governmental entities, healthcare institutions, and community organizations can create holistic solutions that resonate with the needs of diverse populations.
Implementing more robust maternal health initiatives that promote access to quality care before, during, and after pregnancy can pave the way for improved health outcomes. Efforts should be made to educate communities on available resources and support services. Additionally, continuous research and data analysis are critical in tracking maternal health trends over time, enabling the formulation of responsive policies. By continuously advocating for women’s health and striving to eliminate systemic barriers, we can take significant steps towards reducing maternal mortality rates and fostering a healthier future for mothers across the nation.
Frequently Asked Questions
What are the primary factors contributing to the high U.S. maternal mortality rate?
The high U.S. maternal mortality rate can be attributed to a variety of factors including a fragmented healthcare system, inequitable policies, maternity care deserts, and ongoing systemic bias and discrimination against racial and ethnic minorities. Additionally, an increase in chronic health conditions among pregnant individuals contributes to the rate of pregnancy-related deaths.
How do racial disparities in maternal health impact U.S. maternal mortality rates?
Racial disparities in maternal health significantly impact U.S. maternal mortality rates, with American Indian and Alaska Native women experiencing the highest rates of pregnancy-related death. Non-Hispanic Black women also face disproportionately high rates compared to white women, illustrating the urgent need to address inequities within the maternal healthcare system.
What is being done to address preventable maternal deaths in the U.S.?
To combat preventable maternal deaths, there is a growing emphasis on enhancing maternal health care through better quality prenatal and postpartum care. Addressing systemic issues, increasing investment in public health infrastructure, and implementing data-driven policies aimed at reducing disparities are crucial steps being taken.
What role does postpartum care play in reducing maternal mortality in the U.S.?
Postpartum care plays a critical role in reducing maternal mortality in the U.S. As nearly a third of pregnancy-related deaths occur between 42 days and one year after childbirth, improving healthcare access and quality during this extended postpartum period is essential to address health complications that may arise after delivery.
Why is it important to include late maternal deaths in the discussion of U.S. maternal mortality?
Including late maternal deaths in discussions of U.S. maternal mortality is crucial as it sheds light on the ongoing health challenges women face after childbirth. Recognizing that postpartum recovery continues beyond 42 days post-delivery highlights the need for comprehensive care strategies that extend into the first year after giving birth.
What initiatives are being considered to improve maternal health care policies in the U.S.?
Current initiatives aimed at improving maternal health care policies in the U.S. focus on increasing funding for research and public health infrastructure, implementing uniform health policies across states, and promoting innovative healthcare solutions to enhance the quality of care during pregnancy and the postpartum period.
How does the COVID-19 pandemic affect U.S. maternal mortality rates?
The COVID-19 pandemic has contributed to rising U.S. maternal mortality rates, particularly in 2021, as it exacerbated existing healthcare inequities and increased the incidence of chronic health problems that complicate pregnancies. Continued analysis is necessary to understand the full impact of the pandemic on maternal health outcomes.
What steps can individuals take to advocate for maternal health care improvements in the U.S.?
Individuals can advocate for maternal health care improvements by engaging in community initiatives, supporting policy changes that promote equitable maternal health access, and raising awareness of the disparities faced by various racial and ethnic groups within the maternal healthcare system. Participation in advocacy groups and collaboration with healthcare providers can foster positive change.
| Key Points | Details |
|---|---|
| U.S. Maternal Mortality Rate | The U.S. leads high-income countries in maternal mortality, which continues to rise, reaching 32.6 deaths per 100,000 live births in 2022, up from 25.3 in 2018. |
| Preventable Deaths | More than 80% of pregnancy-related deaths are preventable. |
| Racial Disparities | American Indian and Alaska Native women have the highest rate (106.3), followed by Black women (76.9), compared to white women (27.6). |
| COVID-19 Impact | The highest rate increase occurred in 2021, linked to the COVID-19 pandemic. |
| Leading Causes of Death | Cardiovascular disease accounted for over 20% of pregnancy-related deaths. |
| Postpartum Mortality | Late maternal deaths (between 42 days and 1 year postpartum) account for nearly a third of total maternal deaths. |
| Healthcare System Issues | Challenges include a fragmented healthcare system, inequitable policies, and lack of extended postpartum care. |
| Future Recommendations | Increase investment in public health infrastructure and innovative maternal care solutions. |
Summary
U.S. maternal mortality remains a critical public health issue as rates continue to rise, revealing significant disparities linked to race and healthcare access. The findings suggest that with over 80% of maternal deaths being preventable, focused investment in healthcare, particularly prenatal and postpartum care, is essential. Addressing the systemic challenges within the healthcare system could lead to substantial reductions in maternal mortality rates, improving outcomes for mothers across the nation.