Pediatric Cancer Relapse Prediction with AI Technology
Pediatric cancer relapse prediction is a ground-breaking area of research that is transforming the way we approach the treatment of childhood cancers. Utilizing advanced AI techniques, researchers are uncovering new insights into the glioma recurrence risk, which is crucial for improving patient outcomes. A recent study highlights the remarkable ability of an AI tool to analyze multiple brain tumor imaging scans over time, allowing for more accurate predictions than traditional methods. This innovation not only provides hope for better management of high-risk pediatric patients but also reduces the stress of frequent imaging for families who face the burden of uncertainty. With the ongoing integration of temporal learning in healthcare, we are on the brink of a new era in pediatric oncology that could dramatically shift standards of care.
The prediction of cancer return in children, especially in cases involving brain tumors like gliomas, is gaining traction in medical research. By leveraging artificial intelligence in pediatric oncology, specialists are honing in on glioma recurrence risk to enhance treatment strategies. This evolving field, often referred to as brain tumor AI predictions, encompasses innovative approaches such as temporal learning in healthcare, aiming to provide more tailored and effective interventions. With advanced imaging techniques at the forefront, medical practitioners are now better equipped to handle the complexities of childhood cancer imaging and improve life-saving outcomes.
The Role of AI in Pediatric Cancer Management
Artificial intelligence (AI) is revolutionizing the landscape of pediatric cancer management by enhancing diagnostic and predictive capabilities. With machine learning algorithms processing vast amounts of data, healthcare providers can ascertain patient outcomes more definitively than ever before. The advanced predictive analytics provided by AI, particularly in the realm of pediatric gliomas, allows clinicians to make timely decisions that can vastly improve children’s care. Thus, integrating AI in healthcare not only optimizes treatment plans but also minimizes the anxiety that families face when dealing with prolonged follow-up processes.
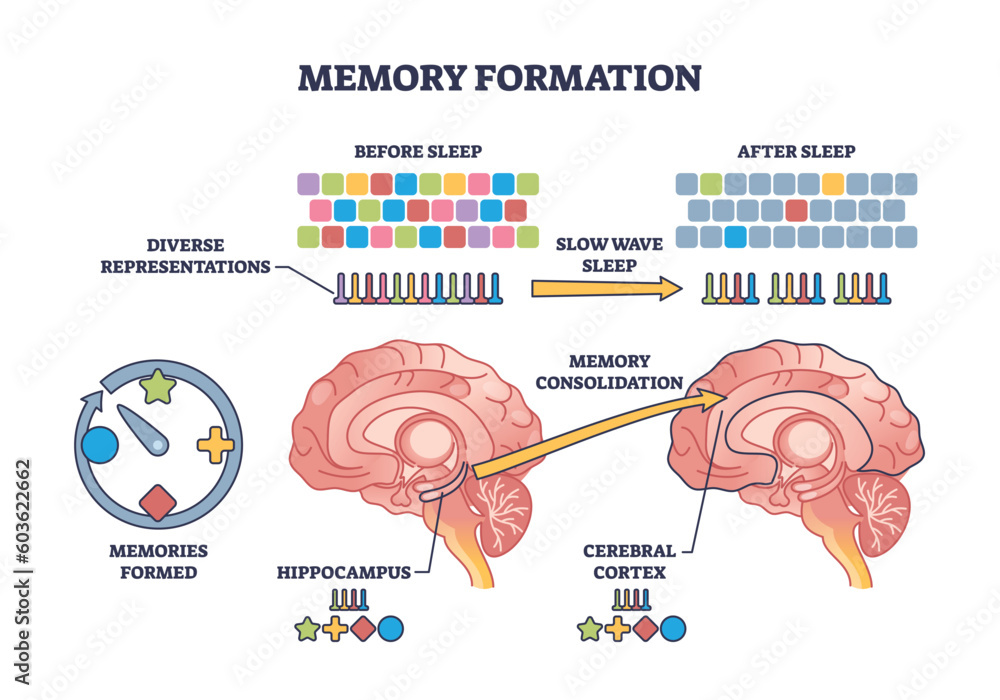
AI’s ability to analyze complex imaging data enables the detection of subtle changes in a child’s health that may indicate the risk of recurrence. By utilizing methods like temporal learning, which examines sequences of images over time, these sophisticated AI systems can provide insights that traditional methods overlook. This predictive capability directly supports targeted interventions, thus improving survival rates and quality of life for pediatric patients battling cancers like gliomas.
Pediatric Cancer Relapse Prediction: A Breakthrough
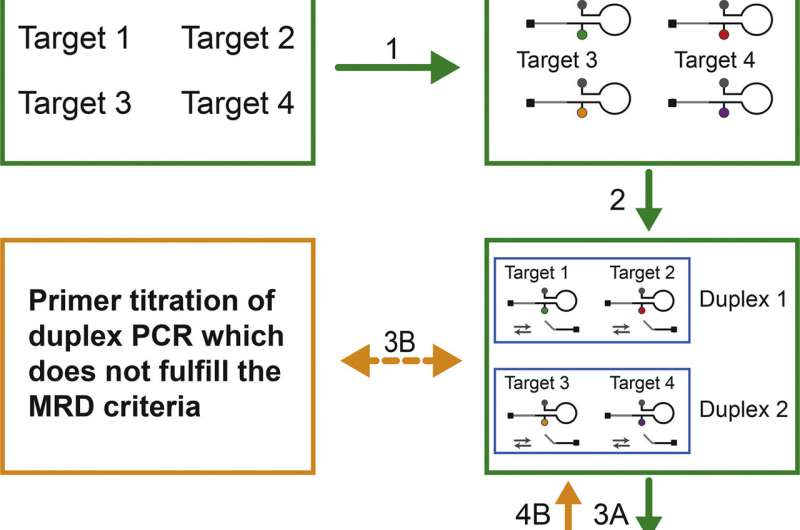
Predicting relapse risk in pediatric cancer patients has historically been fraught with uncertainty, making AI’s recent advancements particularly crucial. The recent study from researchers at Mass General Brigham demonstrates that an AI tool can outperform traditional prediction methods, enhancing the ability of clinicians to identify children at risk of cancer recurrence. By processing multiple magnetic resonance imaging (MRI) scans, the AI model significantly boosts the accuracy of relapse predictions—finding an accuracy range of 75-89%. Such breakthroughs symbolize a vital shift in how medical professionals manage childhood cancers.
Using advanced algorithms that factor in temporal learning from collected scans, the AI tool discerns patterns associated with relapse risks. This method contrasts sharply with previous strategies that relied on isolated images, leading to probabilities of just 50%—no better than chance. The implications are profound; early and accurate predictions through AI will enable healthcare providers to customize patient monitoring and treatment protocols, potentially reducing unnecessary interventions and bolstering early initiatives for those identified as high-risk.
Temporal Learning: Enhancing Predictive Accuracy in Healthcare
Temporal learning represents a seismic shift in predictive modeling, especially within the framework of pediatric oncology. Unlike conventional prediction methods that primarily analyze single snapshots of the disease’s progression, temporal learning synthesizes insights from countless sequential scans. This comprehensive analysis generates a more nuanced understanding of each patient’s journey, providing targeted insights that can predict outcomes more reliably. Such innovation is particularly critical for conditions like gliomas, where timely intervention can be the cornerstone of effective treatment.
In practice, this means that healthcare teams can be proactive rather than reactive. By leveraging temporal learning, providers can immediately recognize changes that signify rising risks of recurrence, consequently triggering discussions for necessary adaptations in treatment plans. This strategic approach not only facilitates better patient outcomes but also opens pathways for further research into AI applications across broader fields of healthcare, including chronic illnesses and preventive medicine.
Advancements in Imaging Technology for Childhood Cancer
Imaging technology is pivotal in the ongoing battle against childhood cancers, enabling early detection and continuous monitoring of tumor progression. Recent advancements in MRI technology have allowed for higher-resolution imaging, which when paired with AI analytics, significantly enhances the evaluation process for conditions like gliomas. These developments afford healthcare providers detailed views of tumors, helping them devise effective treatment strategies while also tracking changes that may indicate a potential relapse.
Moreover, integrating AI into childhood cancer imaging practices has resulted in more precise interpretations of imaging data. With algorithms designed to learn from vast datasets, such technologies keep progressing, potentially revolutionizing how clinicians respond to imaging signals. The promise of AI-powered imaging signals a new era where treatment can be tailored more accurately, offering hope for improved survival rates and quality of life for pediatric patients facing cancer.
AI’s Impact on Brain Tumor Predictions
The impact of AI on brain tumor predictions, particularly concerning pediatric patients, cannot be overstated. Traditional methods have been challenged by their inability to provide timely and accurate predictions regarding glioma recurrence risks. As demonstrated by recent studies, AI models leveraging temporal learning and extensive imaging datasets can now predict patient outcomes at rates significantly exceeding historical norms. This paradigm shift is poised to reshape care delivery in pediatric oncology, addressing unmet clinical needs for accurate relapse risk assessments.
As AI continues to refine its predictive capabilities, it also holds promise for enhancing decision-making processes for both providers and families. By delivering reliable predictions, AI tools can guide the frequency of imaging needed for surveillance, eliminating unnecessary procedures for low-risk patients while ensuring rigorous monitoring for those at higher risk. This data-driven approach empowers families and healthcare professionals with actionable insights, fostering informed discussions about care choices and strategies.
Longitudinal Studies and AI in Healthcare
The integration of longitudinal studies in recent research underscores the importance of examining patient data over time—especially in pediatric oncology. Longitudinal studies involve monitoring patients repeatedly over an extended period, providing rich datasets that fuel AI systems with contextually relevant information. In pediatric cancer care, this method allows for tracking the progression or regression of tumors throughout treatment and recovery, ultimately leading to better-informed predictions about risks, including relapse.
AI’s capacity to process such longitudinal data enhances its learning and predictive accuracy. With applications in situations that necessitate regular imaging—such as brain tumor assessments in children—the insights gained can significantly influence clinical protocols. By drawing on patterns and trends observed across numerous cases, AI can guide tailored approaches that accommodate the unique journeys of each young patient, ensuring that care is both responsive and effective.
Machine Learning and Imaging in Childhood Cancer
The intersection of machine learning and advanced imaging modalities is revolutionizing the realm of childhood cancer diagnosis and treatment. By enabling the analysis of complex imaging data from multiple angles, machine learning algorithms can highlight areas of concern that may be overlooked by human eyes. This technological synergy is particularly noteworthy in pediatric glioma cases, where determining the urgency of interventions can have lasting impacts on outcomes.
As machine learning continues to innovate, healthcare providers gain powerful tools that increase efficiency and accuracy in diagnostic processes. By helping to track tumor changes and correctly predict relapse risks, these systems ensure that children receive timely interventions. The potential for machine learning to enhance the diagnostic process marks a significant advancement in childhood cancer care, making it an invaluable asset in treating rising numbers of pediatric patients.
Implications of AI for Future Pediatric Cancer Research
The implications of adopting AI technologies into pediatric cancer research are profound, offering a new frontier for advancements in medical science. Future research initiatives may leverage AI-driven insights to devise clinical trials aimed at validating the effectiveness of tailored treatment protocols for pediatric patients. By predicting outcomes with greater accuracy and lowering the incidence of relapses, AI paves the way for more targeted therapies that consider individual patient profiles and needs.
Moreover, as collaborations between research institutions and technology companies strengthen, the landscape of pediatric oncology could see a marked transformation. With a focus on developing AI capabilities, researchers could uncover new patterns of disease that enhance understanding of childhood cancers. This data-centered approach not only fosters innovation but may also contribute to global efforts around cancer research, making strides toward curing childhood cancers and improving patient outcomes.
The Future of Pediatric Oncology: AI Innovations
The future of pediatric oncology is inherently tied to innovations in artificial intelligence and machine learning. As researchers continue to unveil the potential of AI tools—especially in predicting pediatric cancer relapse—it is clear that these technologies will greatly influence how healthcare professionals treat young patients. From enhancing diagnostic accuracy to developing personalized treatment protocols, the integration of AI stands to reshape the future trajectory of cancer care for children.
Furthermore, by harnessing the capabilities of AI to process multifaceted data from imaging, genetic profiles, and treatment histories, pediatric oncologists may unlock new possibilities for combating cancer. The resulting advancements will not only improve survival rates but also diminish the associated long-term impacts of childhood cancer treatments. As evidence of AI’s effectiveness grows, it is likely to become a cornerstone in the realms of pediatric healthcare, driving innovation, and improving the quality of life for children battling cancer.
Frequently Asked Questions
What is pediatric cancer relapse prediction and why is it important?
Pediatric cancer relapse prediction refers to the ability to identify the likelihood of cancer returning in children after treatment. This is especially crucial in managing conditions like brain tumors, including gliomas, which can vary significantly in recurrence risk. Accurate predictions can help tailor follow-up care and reduce unnecessary stress on families.
How does AI improve pediatric cancer relapse prediction compared to traditional methods?
AI enhances pediatric cancer relapse prediction by analyzing vast amounts of data, specifically multiple brain scans over time, to identify patterns and subtle changes indicative of possible relapse. Unlike traditional methods, which may rely on single scans with lower accuracy, AI tools can achieve 75-89% accuracy by using temporal learning techniques.
What role does temporal learning play in predicting pediatric glioma recurrence risk?
Temporal learning plays a critical role in predicting pediatric glioma recurrence risk by enabling AI models to analyze sequences of brain scans taken at different time points. This approach helps the algorithm recognize changes that may signal a relapse, providing a more comprehensive understanding of a patient’s health over time.
What are the potential benefits of using AI for brain tumor predictions in children?
The potential benefits of using AI for brain tumor predictions in children include improved accuracy in identifying relapse risk, which could lead to more personalized treatment plans and reduced need for frequent imaging. This can alleviate the emotional burden on families and help healthcare providers make timely interventions.
Why are traditional imaging methods insufficient for predicting cancer relapse in pediatric patients?
Traditional imaging methods often rely on single brain scans, which provide limited information and can result in predictive accuracy as low as 50%. This makes them less effective for identifying subtle changes in a patient’s condition over time, whereas AI-driven approaches analyze multiple images to enhance prediction capabilities.
What are gliomas, and how does AI assist in predicting their recurrence in children?
Gliomas are a type of brain tumor that can occur in children, and their recurrence risk can vary. AI assists in predicting glioma recurrence by analyzing multiple MR scans over the course of treatment, utilizing temporal learning to detect patterns that traditional methods may miss, thus improving outcomes for pediatric patients.
What future developments can we expect in pediatric cancer imaging and AI predictions?
Future developments may include larger-scale clinical trials to validate AI-driven predictive models in diverse healthcare settings. Researchers hope to refine these tools further and integrate them into standard care, optimizing monitoring strategies for pediatric cancer patients and potentially implementing targeted therapies based on individual risk assessments.
How might AI influence the frequency of imaging for pediatric cancer patients?
AI could significantly influence the frequency of imaging by allowing clinicians to better identify low-risk patients who may require less frequent follow-up scans. This targeted approach could minimize the emotional and logistical burden on families while ensuring that high-risk patients receive appropriate monitoring and care.
What are the implications of AI in pediatric cancer care beyond relapse prediction?
The implications of AI in pediatric cancer care extend beyond relapse prediction, potentially improving overall diagnostic accuracy, tailoring treatment plans, and enhancing monitoring protocols. AI technologies may also apply to various aspects of pediatric oncology, including improving imaging techniques and personalizing patient management strategies.
| Key Points | Details |
|---|---|
| AI Tool for Relapse Prediction | An AI tool has shown greater accuracy in predicting relapse risk in pediatric cancer patients, especially for brain tumors. |
| Study Conducted | The study involved researchers from Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, published in The New England Journal of Medicine AI. |
| Temporal Learning Technique | This innovative AI method analyzes multiple brain scans over time to learn and predict when cancer might recur. |
| Prediction Accuracy | The temporal learning model predicted glioma recurrence with an accuracy of 75-89%, significantly better than the 50% of traditional single-image assessments. |
| Future Applications | There is potential for clinical trials to validate AI predictions to improve patient care, including tailored treatment strategies. |
Summary
Pediatric cancer relapse prediction has seen significant advancements through innovative AI technology. The implementation of AI models that utilize temporal learning from multiple brain scans can provide more accurate assessments of relapse risks in pediatric patients with gliomas. As research progresses, we anticipate that these developments will lead to more effective and individualized treatment approaches, ultimately enhancing care for children battling cancer.